Written by Jennifer N. Wu, MD and Roger K. Low, MD
University of California, Davis, Sacramento, CA.
Obesity is a leading public health epidemic with the prevalence in the United States exceeding 30% in most sex and age groups.1 Interestingly, the incidence of urolithiasis has also been on the rise. There is increasing evidence supporting a link between obesity and kidney stones. Historically, this increased risk was thought due to dietary overindulgence leading to increase levels of urinary calcium, oxalate, and uric acid. Recent evidence suggests that other factors may be involved that increase the risk of stones in obese patients. Metabolic syndrome, commonly associated with obesity, has been shown to alter acid base metabolism in the kidney. Metabolic syndrome has been linked with unduly acidic urine and an increased propensity in forming uric acid stones.2
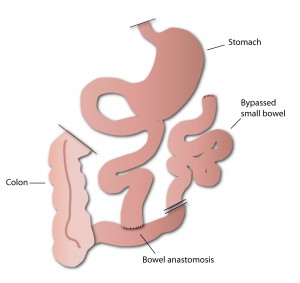
The treatment of obesity has also been associated with an increased risk for forming kidney stones. Surgical intervention is an accepted therapeutic alternative to diet for morbidly obese patients and those with medically complicated obesity. Jejuno-ileal bypass popularized in the 1970’s as a form of surgical treatment for obesity was banned due to patients developing kidney stones and kidney failure. Newer laparoscopic gastric bypass techniques are now commonly performed to treat morbid obesity. 3
Modern day bariatric procedures differ from historical jejuno-ileal bypa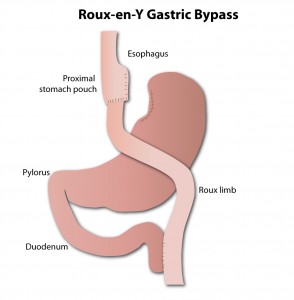 ss procedures in that they bypass smaller lengths of intestine resulting in fewer metabolic consequences. Recent evidence suggests laparoscopic gastric bypass surgery may also be associated with an increased risk of forming kidney stones. Matlaga et al4 evaluated a large cohort of 4,639 patients undergoing gastric bypass surgery and showed 7.65% of these patients developed stones compared to 4.63% of patients not having surgery.
ss procedures in that they bypass smaller lengths of intestine resulting in fewer metabolic consequences. Recent evidence suggests laparoscopic gastric bypass surgery may also be associated with an increased risk of forming kidney stones. Matlaga et al4 evaluated a large cohort of 4,639 patients undergoing gastric bypass surgery and showed 7.65% of these patients developed stones compared to 4.63% of patients not having surgery.
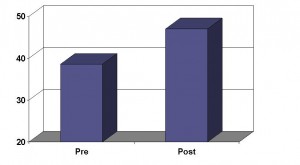
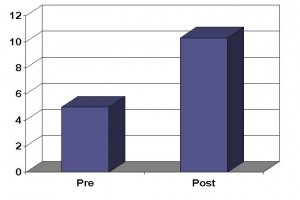
At the University of California, Davis, we recently completed a study evaluating patients’ urine before and after gastric bypass surgery. The results of this study demonstrated increased levels of urinary oxalate and changes in urinary milieu predisposing patients to forming calcium oxalate stones. Our study corroborates other studies demonstrating similar findings.
Patient’s long term risk of developing stones and the impact on kidney function is unknown. Preoperative counseling of patients of their risk of forming stones and dietary counseling postoperatively is warranted. Encouraging adequate hydration and possibly the use of supplemental calcium may be helpful in reducing the risk of stone formation following surgery.
More recent techniques used to treat obesity such as gastric banding and sleeve procedures appear not to be associated with an increased risk of kidney stones. Regardless of the type surgery performed, obese patients should be encouraged to maintain adequate hydration and limit the amount of sodium in their diets.
References:
1. Flegal, K. M., Carroll, M. D., Ogden, C. L. et al.: Prevalence and trends in obesity among US adults, 1999-2008. Jama, 303: 235
2. Asplin, J. R.: Obesity and urolithiasis. Adv Chronic Kidney Dis, 16: 11, 2009
3. Santry, H. P., Gillen, D. L., Lauderdale, D. S.: Trends in bariatric surgical procedures. Jama, 294: 1909, 2005
4. Matlaga, B. R., Shore, A. D., Magnuson, T. et al.: Effect of gastric bypass surgery on kidney stone disease. J Urol, 181: 2573, 2009
I have heard that people who undergo gastric banding procedure (commonly referred to as Lap Band), actually see a decrease in kidney stone episodes compared to patients who have had the gastric bypass procedure. I would love to know if any recent studies have been done as I am scheduled to have the gastric band put on in just a couple of weeks. I am not sure what kind of stones I am passing, but I have had 4 episodes within the past 12 months. The most recent found me hospitalized for 8 days due to a kidney infection that spread to my blood. They put a stent in to hold the stones back while the infections cleared. I have 3 stones, one large one, about 12mm. They will blast them. Hopefully all stones will pass and the stent can be removed soon. It might be wishful thinking and the Lap Band is no magic bullet, but it would be a medical miracle if it helps me. I meet with the bariatric surgeon for the first time since being hospitalized, but all three of my urologists are in agreement that I should continue with my plans for bariatric surgery. Has anyone had a similar experience?