Computerized tomography scanning (CT scans or “cat scans”) have revolutionized the ability of physicians to diagnose kidney stones and has resulted in the vast majority of kidney stones nowadays being correctly diagnosed-the important first step in planning the best treatment option.
However, there is now an increasing awareness among the medical community and public that the use of ionizing radiation (which includes CT scans, plain x-rays, and nuclear scans) carry some risks to individual patients. Being exposed to extremely high doses of radiation on a short term basis usually only occurs during radiation accidents and in these instances can lead to radiation sickness and acute problems requiring hospitalization (such as was the case with some workers at the Japan’s Fukushima Daiichi nuclear reactors). For the majority of patients however, the risk of radiation from imaging studies is related to cumulative small exposures over time that, if excessive, can slightly increase the risk of developing illnesses in the future, including cancer or leukemia.
This is not to say that imaging studies should never be used. Almost every treatment or test used in medicine carries some risk that must be weighed against its benefits. Importantly, not doing an imaging study also can carry risk. If a stone is misdiagnosed, a patient may not receive appropriate treatment or undergo the wrong treatment. Missing a diagnosis of an infected stone can in some cases be life-threatening and prior to the availability of CT scans, some patients experiencing pain from a right sided kidney stone could be misdiagnosed as having appendicitis and undergo an unnecessary appendectomy surgery.
Recommended annual radiation totals
Exposure to radiation is measured in units of milliseverts (mSv). Although no formal recommendations exist for patients, there are established limits for radiation workers (x-ray technicians, physicians) which can be used to estimate recommended patient exposure. The limits for radiation workers are 100 mSv every five years, or 20 mSv per year, averaged over five years. The maximum dose in any one one year recommended is 50 mSv. In a recent journal article, the authors used the totals listed below to categorize patient exposure into low, moderate, high, and very high. However, the use of strict limits for radiation exposure in patients is not supported by the International Commission on Radiological Protection (ICRP) because imaging studies are often used for urgent medical issues that outweigh the potential long-term risk of radiation.
Categories for patient annual radiation exposures
Low Dose (≤3 mSv/yr)
Moderate Dose (>3–20 mSv/yr)
High Dose (>20–50 mSv/yr)
Very High Dose (>50 mSv/yr)
What is the actual risk from medical imaging radiation?
While most researchers agree that excess exposure to low level radiation does increase the risk of developing cancers, translating this into a reliable “number” has been difficult because the increased risk is usually quite low. Some experts do not feel that a real increase in risk occurs below 100 mSv while other experts feel that there is a slight increase in risk from any level of exposure. One estimate that has been used is a 5% increased risk of cancer from 1000 mSv of exposure. Given that the natural occurrence of cancer deaths is actually high, at about 25%, a slight change in this number has been difficult to detect. Despite this, some authors had initially estimated that in the United States CT scans may be the cause of 0.4 to 2.0% of all new cancers. Recently, an updated lower estimate of 0.02-0.04% has been reported.
Annual Background radiation
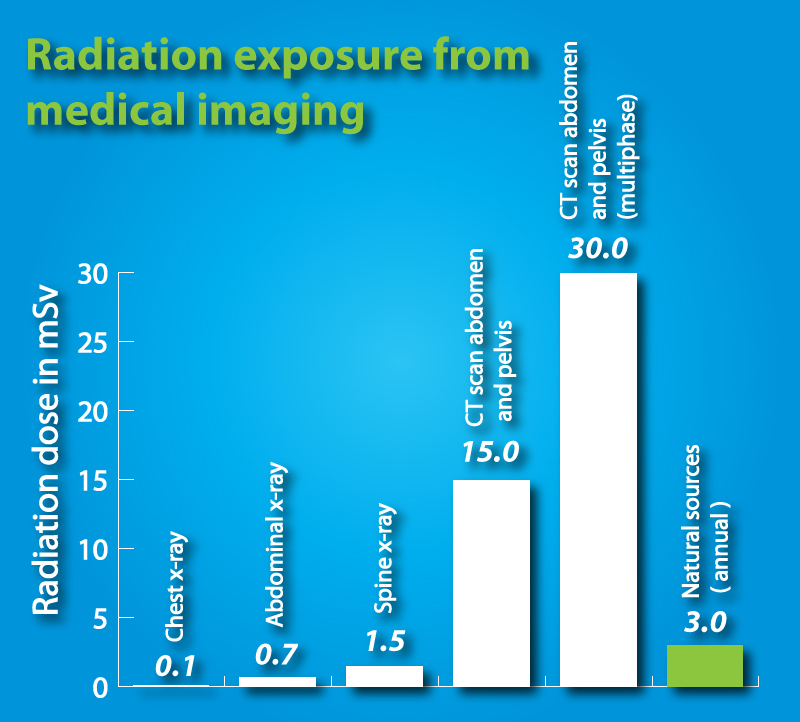
Not many people are aware that everyone experiences radiation exposure from natural sources even without undergoing imaging studies. The total radiation that most individuals experience over the course of a year in the United States is 3 mSv, as estimated by the American College of Radiology and the Radiological Society of North America on their website RadiologyInfo.org. The amount of natural radiation a person is exposed to varies with location and altitude. The breakdown for the state of Colorado is shown below.
Source Dose
Cosmic radiation 0.5 mSv
Terrestial radiation 0.49 mSv
Radon 3.01 mSv
Total 3.86 mSv
Radiation exposure from common studies
The most common study used to diagnose a kidney stone are CT scans, which are very accurate at detecting a stone, its size, and its location. The other common study for kidney stones are plain x-rays of the abdomen, known as “KUB’s” which stands for “kidney, ureter, bladder”. Ultrasound is a third option. It does not use any radiation but is not as effective for detecting stones as a CT scan. It can however easily detect the hydronephrosis, or swelling in a kidney, which a stone can cause. Magnetic resonance imaging studies, or MRI’s, also do not use radiation but are relatively inaccurate for diagnosing kidney stones.
Effective Dose Study
0.7 mSv Abdominal KUB
8 mSv CT abdomen
6 mSv CT pelvis
15 mSv CT abdomen and pelvis combined
________________________________________
0.1 mSv Chest x-ray
0.4 mSv Mammogram
1.5 mSv Spine x-ray
30 mSv CT abdomen and pelvis, multiple phases
Approaches to decreasing radiation exposure
The use of all medical imaging that involves radiation exposure is guided by the principle of “ALARA” or “as low as reasonably achievable”, which recommends that the minimum radiation necessary is used in any clinical situation. One way of decreasing radiation is to use imaging studies that use less radiation, including plain radiographs or ultrasound. However, these alternative studies are not as accurate at detecting kidney stones or correctly determining their size and location than are CT scans. Accurate information is sometimes essential to insure that the right treatment option is chosen, especially when surgery is considered. Therefore, CT scans remain the standard study for the diagnosis of kidney stones. Another proposed method to decrease patient radiation exposure is through the use of “low dose” CT scans, which can reduce total exposure by 80%. Low dose CT scans are equally accurate for large stones but are less accurate at detecting small stones as compared to regular dose CT scans.
In summary, the use of medical imaging for kidney stones, primarily CT scans, has significantly improved the quality of care for kidney stone patients by allowing rapid and accurate diagnosis. However, the use of CT scans and other x-rays do carry a small risk related to the radiation exposure experienced by patients. Using the smallest amount of medical imaging radiation possible is recommended, taking in consideration the need for obtaining an accurate diagnosis.
References
Brenner DJ and Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med 2007; 357: 2277-84.
Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ and Nallamothu BK. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361: 849-57.
Kim BS, Hwang IK, Choi YW, Namkung S, Kim HC, Hwang WC, Choi KM, Park JK, Han TI, Kang W. Low-dose and standard-dose unenhanced helical computed tomography for the assessment of acute renal colic: prospective comparative study. Acta Radiol. 2005 Nov;46(7):756-63.
Dauer LT, Brooks AL, Hoel DG, Morgan WF, Stram D, Tran P. Review and evaluation of updated research on the health effects associated with low-dose ionising radiation. Radiat Prot Dosimetry. 2010 Jul;140(2):103-36. Epub 2010 Apr 22.
Lin EC. Radiation risk from medical imaging. Mayo Clin Proc. 2010 Dec;85(12):1142-6
Moeller DW, Sun LS. Comparison of natural background dose rates for residents of the Amargosa Valley, NV, to those in Leadville, CO, and the states of Colorado and Nevada. Health Phys. 2006 Oct;91(4):338-53.
Herts, B. Risk of Imaging and Monitoring Patients with Urologic Cancers. Plenary lecture, American Urological Association Meeting 2011. Washington, DC.
How much radiation is there from a lithotripsy procedure?
i want all xray images with exposures
[…] Radiation exposure from x-rays or CT scans used to diagnose a stone is more of a risk to the fetus during the first trimester. While the risk is lower during the second and third trimester, experts do not agree on whether there is a “safe” level or radiation and the philosophy of avoiding unnecessary radiation and minimizing it when it is unavoidable is advisable. This strategy includes using ultrasound or MRI initially to establish a diagnosis. However, these studies are not as accurate as CT for the diagnosis of stones. Because an undiagnosed stone can carry its own risks to the mother and fetus (pain, infection, preterm labor, and hypertension), in certain cases, the risk of obtaining imaging in order to treat a stone may be justified. Low dose CT scan protocols or plain x-rays may be used in these situations to still limit the amount of radiation exposure. […]
Thanks so much for this ‘plain english’ explanation of how much radiation I can be exposed to with a CT scan. It was very helpful to me in discussing a plan of care with my doctor during a recent work up that included multiple CT scans and other studies.